|
|
|
You can get e-magazine links on WhatsApp. Click here
|
|
|
|
|
|
Choline: Nutritional shield against non-alcoholic fatty liver disease
|
|
Wednesday, 26 March, 2025, 16 : 00 PM [IST]
|
|
Prarthana Sindhe, Roopa B Patil and Babu RM Ray
|
Have you ever heard of choline? While vitamins and minerals often steal the spotlight in discussions about nutrition, choline remains an underrated yet essential nutrient that plays a crucial role in our health. Recent research has uncovered its remarkable ability to prevent and manage Non-Alcoholic Fatty Liver Disease (NAFLD)—a condition that is fast becoming a global health concern.
Non-alcoholic fatty liver disease or NAFLD (also referred to as metabolic dysfunction-associated steatotic liver disease, or MASLD) is a chronic condition that develops due to an excessive accumulation of fat in the liver. It is usually seen in people who are overweight or obese. It is a heterogeneous disorder that encompasses a range of liver diseases with varying degrees of severity, clinical characteristics, and outcomes. NAFLD is the liver component of a cluster of conditions that are associated with metabolic dysfunction. NAFLD is defined by the presence of steatosis in more than 5% of hepatocytes in association with metabolic risk factors (particularly, obesity and type 2 diabetes) and in the absence of excessive alcohol consumption (=30 g per day for men and =20 g per day for women) or other chronic liver diseases.  The hallmark of NAFLD is hepatic steatosis, but the disease also encompasses non-alcoholic steatohepatitis (NASH) characterised by hepatic inflammation, hepatocyte damage, and fibrosis, highlighting the potentially progressive nature of the disease. The stage of hepatic fibrosis predicts both overall and liver-related mortality and is the strongest predictor of long-term clinical outcomes, with advanced fibrosis (stages 3 and 4) conveying the highest risk of mortality. In addition, metabolic dysfunctions such as insulin resistance, dyslipidemia, and cardiovascular disease are all associated with hepatic steatosis and seem to be more related to hepatic fat accumulation and NAFLD than obesity status.
Prevalence:
NAFLD has rapidly become the most common liver disease globally and is currently estimated to affect 38% of the global population. According to a recent systemic review and meta-analysis, the global prevalence of NAFLD increased from 25.3% in 1990-2006 to 38.0% in 2016-2019. As the most common chronic liver disease in developed countries, NAFLD affects 20–30% of the general population, 50–70% of diabetic patients, and 90% of morbidly obese individuals. The prevalence of adult NAFLD in India has been reported between 6.7% to 55.1% in 2021. The prevalence of paediatric NAFLD in India varies from 7.3% to 22.4% in the healthy population. It is found to be higher among those with diabetes (55.5% –59.7%), overweight or obesity (64.6% –95%) and metabolic syndrome (73%). The prevalence of prediabetes, diabetes, and metabolic syndrome among adults in India is 19–22%, 15–19%, and 30%, respectively, and is increasing in both urban and rural areas.
Causes of NAFLD: - Obesity can primarily cause NAFLD as excess adipose tissue increases free fatty acid (FFA) release to the liver.
- Insulin resistance leads to increased lipolysis, de novo lipogenesis (DNL), and fat accumulation.
- Type 2 Diabetes Mellitus (T2DM) as it impairs glucose metabolism and worsens liver fat buildup.
- High triglycerides & low HDL cholesterol promote hepatic lipid overload leading to Dyslipidemia
- High-Calorie Diets including excess sugar, refined carbs, and saturated fats promote lipogenesis.
- Hypothyroidism reduces metabolism, increasing fat accumulation in the liver.
- Polycystic Ovary Syndrome (PCOS) is associated with insulin resistance, increasing NAFLD risk.
- Gut Dysbiosis alters short-chain fatty acid production and increases gut-derived endotoxins that trigger liver inflammation.
- Sedentary lifestyle
Fatty liver is graded based on the amount of fat in the liver and the impact on liver health.
Table 1: Grades of NAFLD
Grade
|
%
of steatosis
|
Grade
0
|
No
steatosis
|
Grade
1
|
<
33 %
|
Grade
2
|
33-66
%
|
Grade
3
|
>
66 %
|
Common Symptoms:
- Fatigue – Persistent tiredness or lack of energy
- Discomfort or Pain – A dull ache or discomfort in the upper right abdomen
- Unexplained Weight Loss – Some people may lose weight without trying
- Weakness – General feeling of being unwell or weak
Importance of Choline in NAFLDCholine is a constituent of cell and mitochondrial membranes and of the neurotransmitter acetylcholine. It is a quaternary amine present in all mammalian tissues. It influences diverse processes such as lipid metabolism, signalling through lipid second messengers, methylation-dependent biosynthesis of molecules, activation of nuclear receptors, enterohepatic circulation of bile and cholesterol, plasma membrane fluidity and mitochondrial bioenergetics.
Choline is necessary to maintain normal liver function. It is involved in hepatic secretion of VLDL cholesterol, host–gut microbiota interactions and one-carbon metabolism, all of which underlie the pathogenesis of NAFLD. It is a precursor of phospholipids, phosphatidylcholine, lysophosphatidylcholine and sphingomyelin. Choline is an essential nutrient because its endogenous biosynthesis is generally not sufficient to meet human requirements.
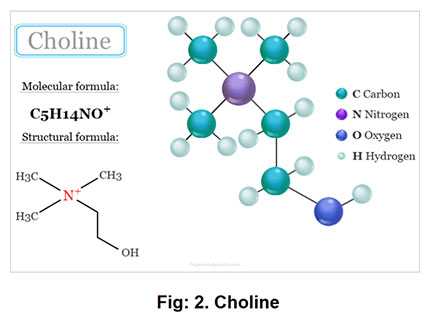
Physicochemical Properties:
- Molecular formula: C5H14NO?
- Highly soluble in water due to its polar nature
- Can degrade under high temperature or in the presence of strong acids or bases
- Found in various dietary forms, including free choline, phosphatidylcholine and glycerophosphocholine
Biological Properties:- Choline is a precursor to phosphatidylcholine, a critical component of cell membranes and sphingomyelin, which is abundant in nerve tissues.
- Involved in one-carbon metabolism, donating methyl groups for processes such as DNA methylation and neurotransmitter synthesis.
- Plays a crucial role in fetal brain development during pregnancy and early childhood.
Functions of Choline: - Choline is necessary to maintain normal liver function. It is involved in hepatic secretion of VLDL cholesterol, host–gut microbiota interactions, and one-carbon metabolism
- It is used to synthesise acetylcholine, a neurotransmitter that plays a role in muscle contraction, memory and neural development
- It helps transport lipids from liver to the circulation via lipoproteins (acts as lipotropic agent)
- Choline is involved in early development of the brain, gene expression, cell membrane signaling, and brain metabolism.
- Choline is vital for neural tube closure during early fetal development, which occurs within the first few weeks of pregnancy. Neural tube defects (NTDs), such as spina bifida are serious birth defects that affect the spine and brain. Adequate choline intake has been linked to a reduced risk of NTDs
- It helps maintain the structural integrity of cell membranes, which affects cell function, activity and size
Effects of Choline Deficiency and Toxicity
Deficiency: - Because of its wide-ranging role in human metabolism, from cell structure to neurotransmitter synthesis, choline deficiency can cause fatty liver, which increases cancer and cardiovascular disease risk.
- It also decreases SAM production, which partakes in DNA methylation – this decrease may also contribute to carcinogenesis
- Choline is in high demand during pregnancy as a substrate for building cellular membranes, raising choline stores in fetal and placental tissues, and for increased production of lipoproteins. Low maternal intake of choline is associated with an increased risk of neural tube defects
Toxicity: - Excessive doses of choline can have adverse effects. Daily 8–20 g doses of choline, for example, have been found to cause low blood pressure, nausea, diarrhoea and fish-like body odour. The odour is due to trimethylamine (TMA) formed by the gut microbes from the unabsorbed choline.
Mechanisms of fat accumulation in the liver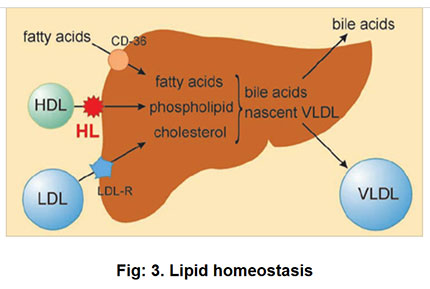 "CD-36" is the primary protein responsible for the uptake of fatty acids from lipoproteins like VLDL, and to a lesser extent HDL, into cells. This process is facilitated by the interaction of CD-36 with the fatty acids within the lipoprotein, allowing the cell to absorb them for energy usage. The liver absorbs fatty acids (via CD36) and uses them to create cholesterol, phospholipids, and VLDL, which transport fats to other tissues. Cholesterol is also converted into bile acids for fat digestion. HDL brings cholesterol back to the liver, while LDL delivers it to tissues. The liver regulates lipid levels by recycling or excreting excess cholesterol. - HL (Hepatic lipase) is a factor in hepatic intracellular lipid homeostasis.
- Lipids are taken up by the liver via several mechanisms.
- Lipoprotein receptors mediate in the endocytosis of whole lipoproteins
- HL modulate the binding of lipoproteins (e.g., chylomicron-remnants) to receptors, or stimulate the uptake of HDL-C (ester) directly, or facilitate selective uptake via SR-BI
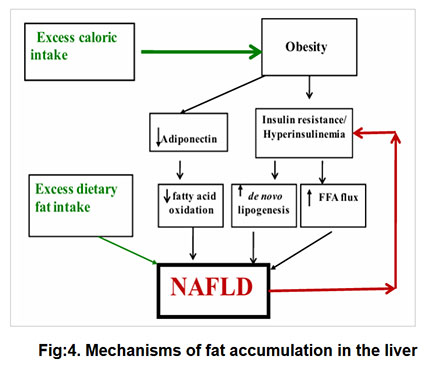 Excess caloric intake plays a central role for inducing obesity and thus contributing to insulin resistance. Obesity may additionally impact fat accumulation in the liver by decreasing adiponectin levels (Adiponectin is a protein hormone that helps regulate glucose levels, fatty acid breakdown and reduce inflammation) and insulin resistance contributes to NAFLD directly by increasing de novo lipogenesis and indirectly by increasing FFA flux to the liver via decreased inhibition of lipolysis. In addition, excess dietary fat intake directly could also contribute to a causal role in hepatic steatosis.
TWO HIT HYPOTHESIS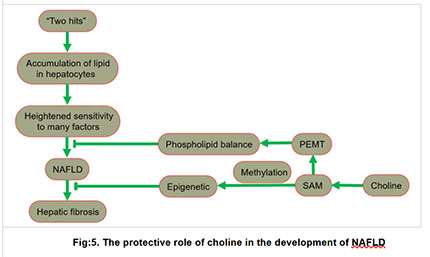 Two Hit Hypothesis- First hit involves the accumulation of lipid in hepatocyte. The increase in lipid uptake, the increase in de novo synthesis of fat, the decrease in lipoprotein synthesis, or the decrease in fatty acid oxidation leads to lipid accumulation.
- Second hit promotes liver cell damage and death, inflammation, activation of hepatic stellate cells (HSCs), and production of extracellular matrix, eventually leading to fibrosis.
Accumulation of lipids in hepatocytesWhen lipids accumulate excessively in the liver, it creates an imbalance, increasing the risk of developing NAFLD.
Heightened sensitivity to many factors
The liver has a heightened sensitivity to many previously inconsequential factors, including gut derived endotoxin, endoplasmic reticulum (ER) stress, oxidative stress and subsequent lipid peroxidation and mitochondrial dysfunction.
Choline's role in NAFLD prevention
- Choline helps regulate several processes to counteract this accumulation and prevent NAFLD progression
- Phospholipid balance: Choline is critical for the synthesis of phosphatidylcholine (a major component of cell membranes) through the enzyme PEMT (phosphatidylethanolamine-N-methyltransferase). Proper phospholipid production helps maintain liver health by facilitating lipid export from the liver.
- Methylation and Epigenetics: Choline acts as a methyl donor via SAM (S-adenosylmethionine), a key compound in methylation reactions. Methylation regulates gene expression (epigenetics), which helps maintain liver function and prevent damage.
Effect of choline deficiency- NAFLD: Without adequate choline, lipid accumulation worsens and the liver's ability to export fat is impaired.
- Hepatic fibrosis: Prolonged lipid accumulation and damage can lead to fibrosis (scarring of liver tissue), worsening the liver's health.
Table 2: RDA of Choline
Men
|
550
mg/day
|
Women
|
425
mg/day
|
Pregnant
|
450
mg/day
|
Lactating
|
550
mg/day
|
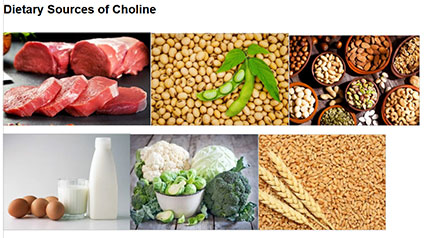 Rich dietary sources of choline include organ meats, egg yolks, dairy products, peanuts, wheat, certain beans, nuts and seeds.
ConclusionCholine is an essential yet often overlooked nutrient that plays a crucial role in preventing and managing Non-Alcoholic Fatty Liver Disease. NAFLD, a growing global health concern, is strongly linked to metabolic disorders such as obesity, diabetes, and insulin resistance. Choline contributes to liver health by facilitating lipid metabolism, preventing fat accumulation, and regulating gene expression through methylation. A deficiency in choline impairs the liver’s ability to export fat, leading to increased risk of hepatic steatosis, fibrosis, and NAFLD progression. Given its importance, adequate dietary intake of choline, through sources such as eggs, dairy, organ meats and certain plant-based foods, is essential for maintaining liver function and overall metabolic health. (Sindhe is PG scholar, Department of Food Science and Nutrition, UAS, GKVK, Bengaluru; Patil is assistant professor, Department of Food Science and Nutrition, UAS, GKVK, Bengaluru; Ray is assistant professor, College of Agricultural Engineering, UAS, GKVK, Bengaluru. They can be reached at prarthanasindhe86729@gmail.com) |
|
|
|
|
|
|
|
|
|